🦶 Heel Pain Holding You Back? Understanding Plantar Fasciitis
Expert Chiropractic Care for Melbourne CBD Runners, Walkers & Office Worker
If you’ve ever stepped out of bed and felt a sharp pain under your heel which may last a few steps or a few minutes, you might be dealing with plantar fasciitis. This pain in the morning is called “start-up pain” and is a hallmark feature of plantar fasciitis. It’s one of the most common causes of heel pain—and one we treat regularly at Shannon Clinic in Melbourne CBD.
🔍 What Is Plantar Fasciitis?
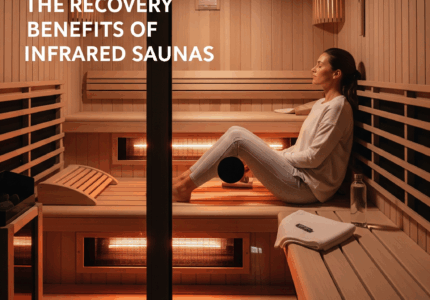
The plantar fascia is a band of dense fibrous tissue or aponeurosis that runs from the medial (inner) aspect of the calcaneus (heel bone) to the forefoot. The fascia runs in three bands (lateral, medial and central) fanning across the sole (plantar aspect) of the foot.
The plantar fascia plays an important role in maintaining, stabilizing and controlling the longitudinal arch which is stressed during locomotion. As well as, aiding in the distribution of weight evenly across the metatarsal heads; while also assisting with efficient propulsion forces, by acting as a cushion for the soft tissues around the metatarsal heads. Therefore, any alterations impacting the fascias ability to maintain the longitudinal arch leads to increased stress loading of the fascial tissues.
⚠️ Symptoms to Watch For

Plantar fasciitis usually presents with focal pain around the heel, accompanied by start-up pain first thing in the morning and/or after sitting for extended periods, as well as pain during walking/running. The pain associated with plantar fasciitis is due to degenerative changes in the fascial tissue, weakening the tissue as a result of excess stress loading. The most commonly involved fascial bands are the medial and central bands.
Diagnosing Plantar Fasciitis
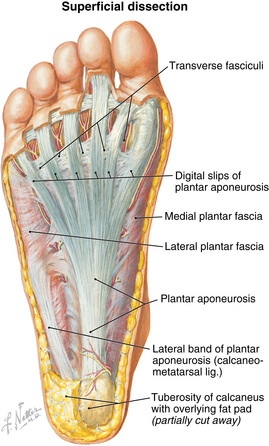
Plantar fasciitis is routinely diagnosed following a thorough history and physical examination by an appropriately trained health or sports practitioner. If further imaging is required, an ultrasound is usually the primary imaging modality, which is capable of showing any thickening, tearing and/or increased vascular flow of the plantar fascia which are hallmark signs of plantar fasciitis, as well as any bone spurs or cysts that may additionally be contributing to the patients heel pain.
What Causes Plantar Fasciitis
Excess stress loading can be multifactorial and can include, direct training or volume load increases, and/or biomechanical imbalances leading to increased tissue loading. Causes can include:
- Acute load spikes (increasing walking/running load too quickly – a classic example being individuals who do not walk much day-to-day (i.e 5k steps per day) but then go on holiday and start walking 15-25k steps per day for 1, 2, 3, 4 weeks in a row.
- Excessive foot pronation – collapsing of the longitudinal arch
- High arches
- Tight achilles, calf, intrinsic foot muscles
- Poor fitting shoes
- Poor gait mechanics – reduced great toe extension, reduced dorsiflexion of the ankle
- High body mass index – placing higher loads over the plantar fascia
🧠 Treatment That Works
There are a wide variety of treatment options available for plantar fasciitis, ranging from over the counter analgesics, to orthotics and night splinting, through to physical therapy, injection interventions and surgery. In this blog the focus will be on the more common treatment interventions.
Orthotics
Orthotics are commonly prescribed for plantar fasciitis with one study indicating they may help reduce pain associated with PF in the medium term. However, in the short and long term there is low quality evidence to suggest orthotics do not provide any improvement in pain. Furthermore, a 2018 systematic review and meta analysis found orthotics were not superior for improving pain and function when compared to sham and other conservative interventions.
Moreover, there is evidence indicating orthotics may lead to a weakening of the intrinsic foot muscles which may potentially augment the already weakened and dysfunctional tissue driving the degenerative changes associated with plantar fasciitis. It is for this reason Melbourne sports chiropractor Dr. Shannon does not advocate the use of orthotics as a front-line intervention for improving pain and function in patients with plantar fasciitis.
Shock-Wave Therapy
Shock-wave therapy is a treatment intervention which has been gaining some traction in recent years. There is evidence to suggest shock-wave therapy may improve pain and function and is ranked as a treatment option most likely to be effective at improving pain and function over the short, medium and long term. Shock-wave therapy is therefore a treatment option that could be considered, particularly in more chronic or recalcitrant cases.
Strengthening/Loading Exercise Programs
The research in this area is currently lacking. One of the difficulties at present is the lack of a standardized strength program which can be used for research purposes. However, in 2023 a consensus paper was released with 3 specific strengthening programs designed to be used in clinical trials. This is an area of most interest as individuals with plantar fasciitis exhibit reduced foot and ankle strength, muscle size and function.
In 2014, a randomized controlled trial comparing stretching and high load strengthening exercises reported a superior self report outcome after 3 months in the strengthening group. This is not surprising, considering plantar fasciitis is associated with degenerative change of fascial tissue, an appearance somewhat similar to tendinopathy which in the case of achilles and patellar tendinopathy, responds well to moderate to heavy strength loading programs.
It is for these reasons the cornerstone to Dr. Shannon’s approach to managing plantar fasciitis includes strengthening exercises, which are combined with load management and correcting any biomechanical imbalances in the lower extremity. As more studies are published exploring strength loading on plantar fasciitis pain and function, it is hoped the results will reflect what is seen in our Melbourne city sports chiropractic clinic.
👉 Learn how the Shannon Clinic manages lateral ankle sprains with sports chiropractic care.
Injection Interventions
At present the pathophysiology of plantar fasciitis is not well understood however, there is histopathological evidence indicating degenerative changes and atrophy of the muscle tissue, together with inflammation either in the fascia or muscle tissue. It therefore would be logical to assume that an intervention which potentially reduces inflammation and aids with tissue repair would perform superior to an intervention which solely focuses on reduction in tissue inflammation. The evidence comparing these two types of injection interventions leans towards supporting this assumption.
The two most prevalent injection interventions for plantar fasciitis are corticosteroid and platelet rich plasma (PRP) injections. Corticosteroid injections (CSI) are a powerful anti-inflammatory intervention that have shown to improve pain levels in the short-term (<3 months) in plantar fasciitis however, they come with risks of tendon ruptures, fat pad atrophy and there appears to be an absence of any medium to long term benefit.
PRP injections possess strong anti-inflammatory properties, in addition to high levels of cytokines and growth factors which are important in wound healing. Furthermore, PRP injections have not been associated with any adverse effects on the plantar tissue. Moreover, they provide better improvements in pain and function than CSI’s over 6 and 12 months and could be considered in chronic cases in conjuction with strength loading interventions.
Surgery
Surgery should only be considered in recalcitrant cases of plantar fasciitis that have failed to respond to conservative management. Procedures include plantar fasciotomy, gastrocnemius release, radiofrequency tenotomy, dry needling. All have been shown to be effective (improving pain and function) over the short and medium term.
Summary
Although futher research is needed to understand the true pathophysiological cause, plantar fasciitis appears to have similar characteristics to tendinopathy such as Achilles tendinopathy including degenerative changes of the tissue due to excess stress loading of the tissue. As the evidence currently shows, treatment interventions which aim to address the degenerative and inflammatory changes in the plantar fascia tissues appear to be more effective at reducing pain and improving function over the medium and long term (6-12 months) over interventions that focus primarily on symptompatic control.
It is for this very reason our approach to treating plantar fasciitis at the Shannon Clinic – Melbourne Chiropractic and Sports Care is to focus on improving the quality and strength of the plantar fascia tissue through a loading program, whilst also addressing any mechanical imbalances and training load problems which may be contributing to the excess stress loading of the plantar fascia. In recalcitrant cases that fail to adequately respond to exercise therapy and load management, we utilize PRP injections to assist with pain management to allow individuals to return to their rehabilitation program.
👉 Read our post on training load and injury prevention to understand how recovery fits into your performance plan.
📍 Visit Shannon Clinic in Melbourne CBD
If you are experiencing plantar fascia pain and would like to make an appointment with Melbourne sports chiropractor Dr. Nicholas Shannon you can book below. If you found this blog of interest, you might enjoy our blog on elbow tendinopathy.